South Sudan: From a snakebite survivor to an active health promoter
In 1 click, help us spread this information :
Around 1.5 billion people worldwide, nearly one fifth of the global population, require medical interventions for neglected tropical diseases (NTDs) every year.
According to the World Health Organization (WHO), there are 21 recognized NTDs, ranging from parasitic and bacterial infections to envenoming. While some progress has been made, particularly in terms of control or near-elimination of few diseases in few countries, in less than half of NTD-endemic countries. Even within these contexts, elimination has been achieved for only one or two diseases out of the 21. Meanwhile, for several NTDs, the situation is worsening due to funding cuts, conflict, and fragile health systems, conflicts, or climate crises.
NTDs are often fatal if left untreated, or they cause severe disfigurement and stigma. They disproportionately affect the most marginalized and displaced communities and frequently trap people in cycles of disability, lifelong suffering, social isolation, and poverty.
Many NTDs cause extreme pain, yet they remain largely overlooked despite their significant morbidity and mortality. Importantly, many of these diseases are preventable or treatable, but continue to be unfairly neglected.
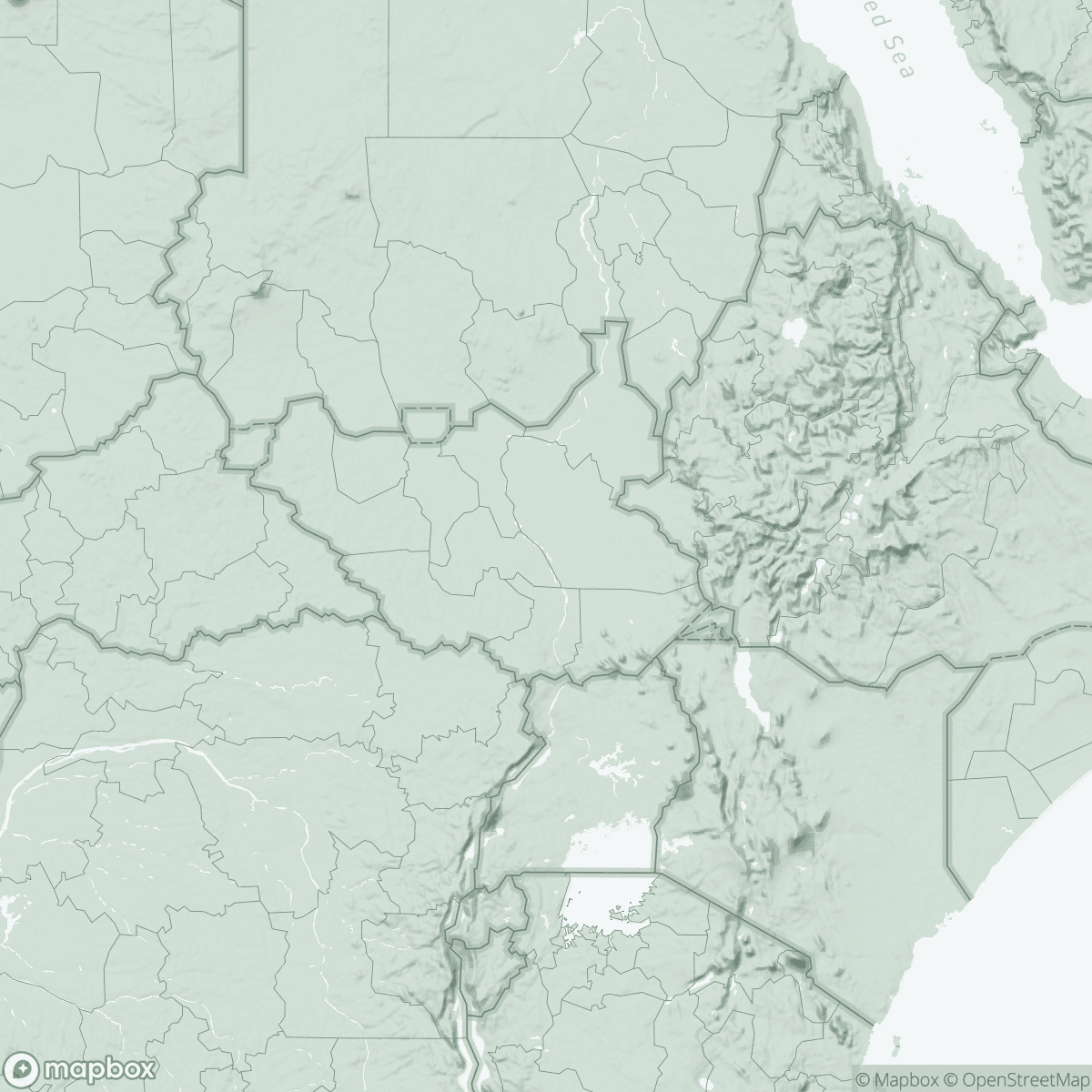
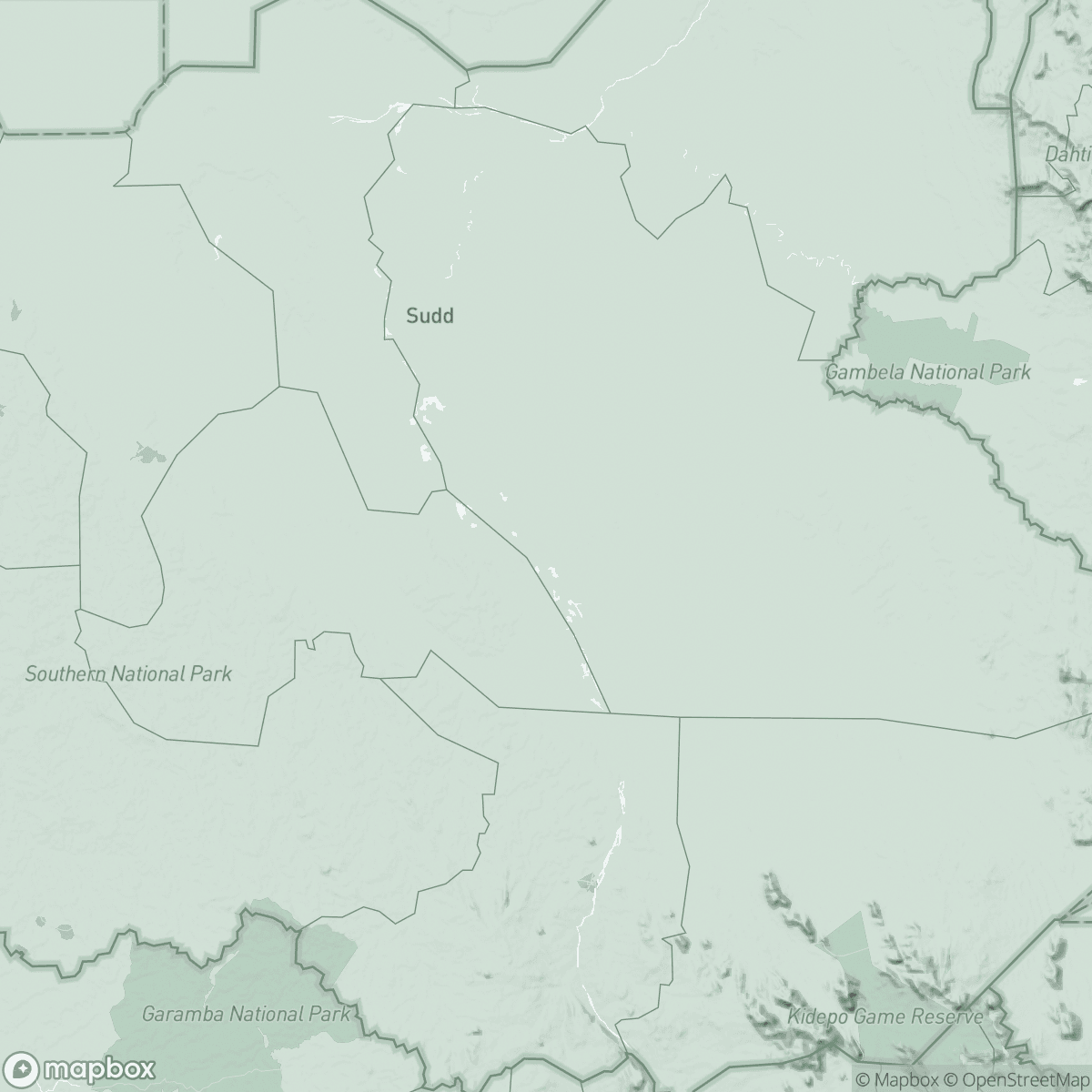
Snakebite is one of this list of neglected tropical diseases and represents a major public health emergency in countries like South Sudan, which has some of the lowest levels of ecological research on snakes, yet reports a high number of snakebite cases.
Between May and October every year, an increasingly risky period due to climate-related changes like floods and heavy rains, MSF teams admit many patients to hospitals suffering from snakebite envenoming.
The following is the testimony of our South Sudanese colleague, Noon Makor Arop, who is working with MSF since 2019. Noon was bitten by a snake in 2021; after receiving treatment, he has been actively working as a Health Promotion and Community Engagement Supervisor in Abyei.
“I have personal experience with snakebites, having been bitten in May 2021. It happened while I was on my way home from the market at 8:00 PM. I didn't realize it was a snake initially, but I soon felt pain and swelling in the bite area. I rushed to the hospital where my colleagues from MSF have been working, and I was treated with antivenom, and I recovered and was discharged.
In my role as a health promoter actively working to raise awareness about the danger of snakebites, I have encountered many patients suffering from snakebites both in hospital and in the community. Some of them have undergone serious surgeries because they arrived late at the hospital, often due to their reliance on traditional treatment methods.

In South Sudan, snakebite is a severe and often fatal health issue that is considered a neglected medical emergency. This situation is exacerbated by extreme environmental conditions and a fragile healthcare system. Snakebite is frequently among the top ten reasons for hospitalization in many hospitals across South Sudan, putting lives at risk. In 2025 alone, MSF treated 197 patients for snakebites in just two hospitals in two areas, including Abyei where I work.
In rural areas, health facilities often do not have high-quality antivenom, which is frequently unavailable or prohibitively expensive. For example, in Abyei, antivenom can only be found at Ameth Bek Referral Hospital, by the support of MSF teams. As a result, many patients miss the “Golden Hour,” which is critical for effective treatment. Additionally, many patients lack access to transportation and live far from hospitals.
Traditional healers often attempt to bridge this gap. Their methods such as cutting the wound or applying “black stones”, often worsen the injury and waste precious time that could be used to save lives. And environmental changes, such as flooding and climate shocks, are forcing snakes into closer contact with human habitats.
On the World Neglected Tropical Diseases Day, I want my words to reach as many people as possible who may read my message. We should avoid relying on traditional remedies for snakebites because they can cause delays in necessary. It is a matter of life or death and so lifesaving conventional treatments and only immediate access to safe, effective, and affordable antivenom can prevent death and severe disability.
As a health promoter, I would give the following tips for those who might fall victims to being bitten by a snake:
To avoid a snakebite:
✓ Use light at night.
✓ Wear closed shoes especially on high grass
✓ If you see a snake, stay calm and move away.
In case of snakebite:
✓ Stay calm, avoid fast motion movement to slow venom spread.
✓ Remove jewelry or tight clothing before swelling occurs.
✓ Immobilize the injured limb with a splint or sling, keeping it at or below heart level.
✓ Get the victim to a health facility quickly.
✓ Do not use a tourniquet; it can cause limb loss.
✓ Avoid cutting, sucking, or icing the wound.
✓ Do not attempt to catch or kill the snake for identification.
Stay safe and always well.”
The World Health Organization estimates that 5.4 million people are bitten by snakes every year.
Around 138,000 people die annually as a result, while nearly three times as many survivors are left with permanent disabilities, including limb loss and long-term physical and psychological consequences.
Snakebite care can be fully integrated into primary and secondary health services, rather than treated as a marginal component of neglected tropical disease (NTD) programs.
Globally, MSF teams treat around 8000 snakebite patients each year.
Strengthening routine health services would allow patients to access care earlier and reduce the burden on overstretched referral hospitals.
Despite having the highest mortality of all 21 NTDs, snakebite envenoming remains severely underfunded and overlooked. Investments in prevention, treatment, and access to safe antivenom are disproportionately low, even though effective solutions exist. Ensuring timely access to quality, affordable polyvalent antivenom, combined with proper clinical training and patient follow-up, would drastically reduce deaths, permanent disabilities, and the need for costly interventions such as intensive care, blood transfusions, surgery, or long-term rehabilitation.
Snakebite deaths and disabilities are largely preventable. What is missing is not the knowledge or the tools, but the political commitment and sustained investment to act now.