“It’s in the psychologist's power to help you find ways to live with trauma”
In 1 click, help us spread this information :
“I've lived in Mariupol ever since I was a child,” says Alina Rosheva. “We had a beautiful house. I had a group of friends. I looked forward to the future with confidence. This all came to an end in February 2022. All of our relatives came to join us in our basement. There were 13 of us, young and old, trying to survive however we could.
The explosions were so loud that the doors to the basement were blown in. The decision to leave was obvious. If we had stayed, we wouldn't be alive.”
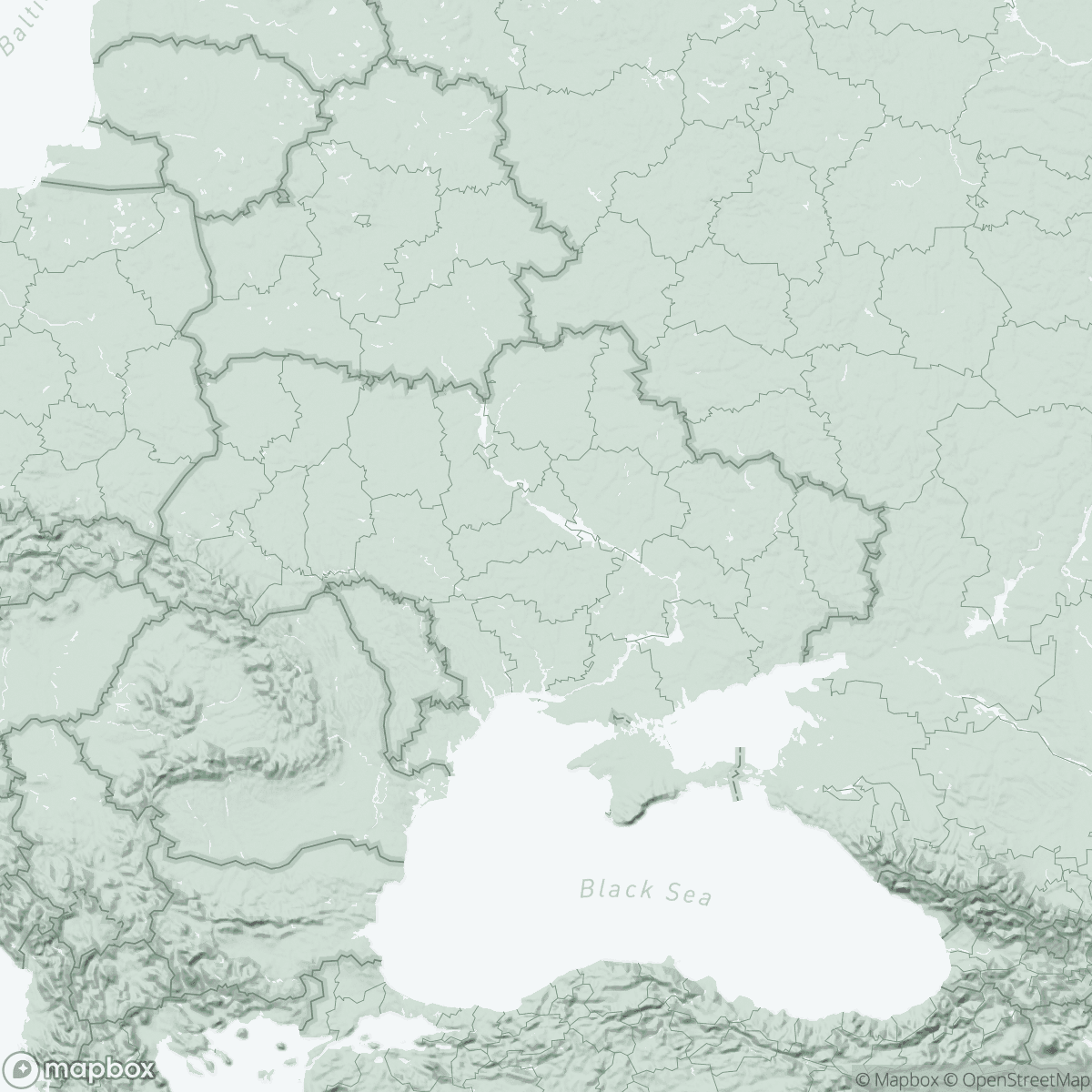
After 20 days sheltering in the basement, 20-year-old Alina undertook a long and dangerous journey with her relatives, passing a dozen checkpoints controlled by the Russian army, before crossing the frontline to reach territory controlled by the Ukrainian army. Heading west, through Zaporizhzhia, she finally reached the city of Vinnytsia, which has become her temporary home.
Like Alina, more than 4.6 million Ukrainians are currently displaced within the country, 160,000 of them in Vinnytsia.
From April 2022, MSF mobile clinics provided medical and psychological first aid in shelters in and around the city where displaced people were staying. To raise awareness of the psychological support on offer, MSF health promoters run group sessions aimed at both adults and children.
The psychological support has made a tangible difference to many people’s lives, especially those of children.
"When we first started, people told us that their children just sat there, not communicating with anyone," said MSF health promoter Mariana Rachok.
We were happy to see that, over time and sessions, the children began to play together."
Mental care for war related trauma
MSF teams in Vinnytsia soon realised there was a need for specialised mental healthcare for people living with post-traumatic stress disorder (PTSD) as a result of the conflict. In September 2023, MSF opened a trauma centre in Vinnytsia for people with war-related PTSD.
“Most of the patients are displaced people who have seen and survived unbelievably horrific events," says MSF doctor Lilia Savchenko. "They experience hopelessness, nightmares, recurrent flashbacks, anxiety and detachment from other people. These are all normal reactions to abnormal events. But if these conditions persist for more than three to six months, then this is an indication that the person has PTSD. From then on, it is likely to get worse every day."
MSF psychologists currently see around 30 patients for weekly consultations.
Patients have an initial assessment, in the form of a consultation with the doctor and one of the psychologists, who make a diagnosis based on tests and clinical observation, and devise a treatment programme.
"The treatment programme depends on the mental state in which the person comes to us, but involve an average of 10-15 consultations," says Dr Savchenko. At consultations, MSF psychologists use evidence-based practice divided into three phases – stabilisation, trauma processing and reintegration into social life – and tailored to patients’ needs.
Stigma around mental healthcare
A common symptom of PTSD is reluctance to seek help. This is often exacerbated by the stigma that exists around mental healthcare.
There is a lack of understanding of how psychotherapy works and this can discourage people from seeking help,” says Andrii Panasiuk, MSF psychologist and mental health supervisor. “This is where raising awareness plays a key role.”
To raise awareness of PTSD and inform people about its symptoms, MSF teams conduct sessions with GPs and with veterans' associations. They also run psychoeducation sessions on the signs of PTSD during creative workshops and art activities with local organisations for displaced people such as I’Mariupol or the Kherson hub. During these activities, health promoters sit and talk with each participant individually, in order to build trust, identify people who could benefit from psychological support and empower them to seek care.
“I often draw parallels between physical and mental injuries,” says Mariana Rachok. “If you don’t disinfect or treat a wound, but simply cover it up and try to ignore it, the wound just gets worse.
It’s not in the psychologist's power to bring back your home or your loved one, but it is in their power to help you find ways to live with trauma, to learn to understand your emotions, to cope with them and to find ways to help yourself.”
Starting to live again

Lidia Bazualyeva, aged 74, was displaced from her home in Kherson and received mental health support from MSF for PTSD.
All these creative activities helped me psychologically, as did the consultation with the psychologist. Slowly I came out of this very difficult post-traumatic state. Now this is my only family and I have never missed an event facilitated by the health promoters”, she says with a smile. “When I communicate and share information, I slowly start to live.”
Alina Rosheva recently completed MSF's PTSD programme. "I went to a lot of therapy sessions,” she says. “It was difficult. Recovery does not happen overnight – it's a long and complicated process.
But three months after I started the treatment, I stopped having panic attacks, they went away. At last I had learned to control them and to deal with them.”
Today, Alina is in charge of organising cultural activities for the I'Mariupol organisation. She has built up a new group of friends in Vinnytsia and is facing the future with confidence again.