A Forgotten Health Emergency
In 1 click, help us spread this information :
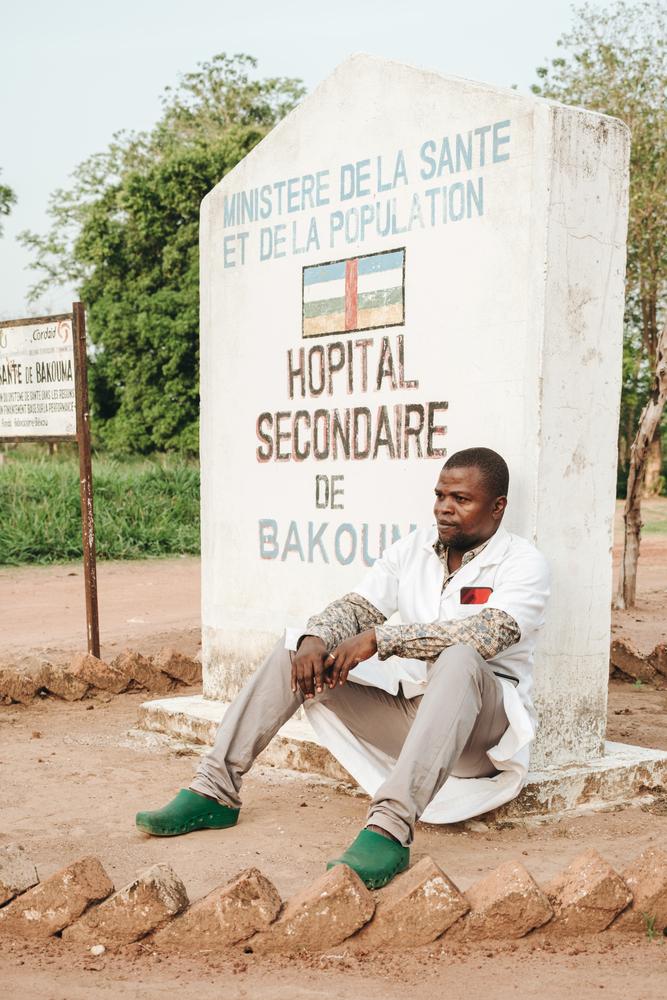
"When I arrived here, I felt like I was falling into a void," said Dr. Louis-Marie Sabio while standing in the courtyard of the Bakouma secondary hospital. At the beginning of 2023, Dr. Sabio — a former MSF doctor in the city of Bangassou — took over the management of the hospital. It is meant to handle surgical complications in a volatile area near Nzacko, in the northwestern part of the Mbomou prefecture.
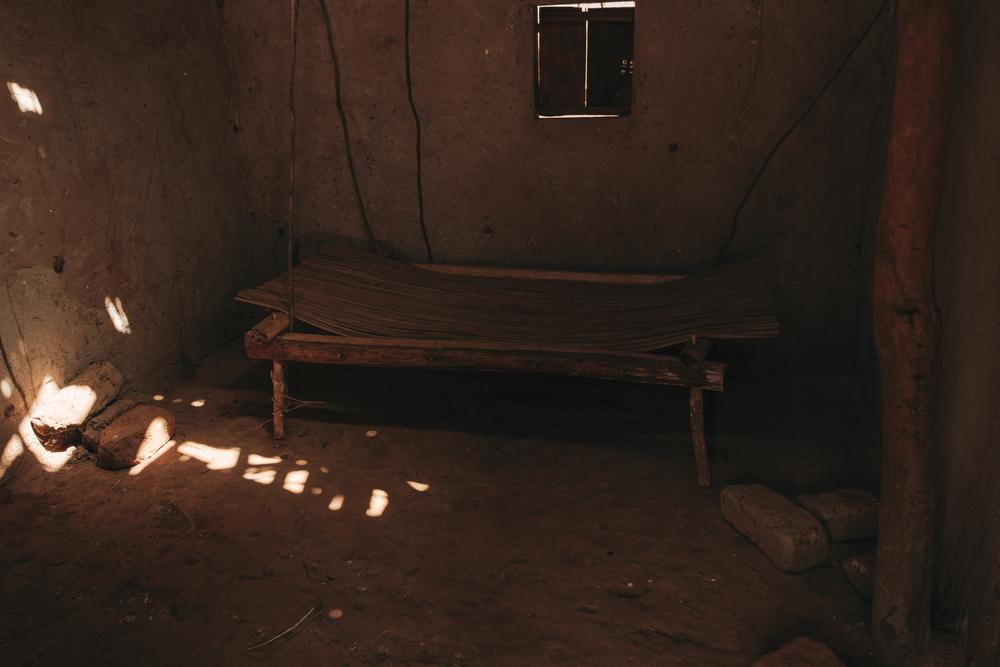
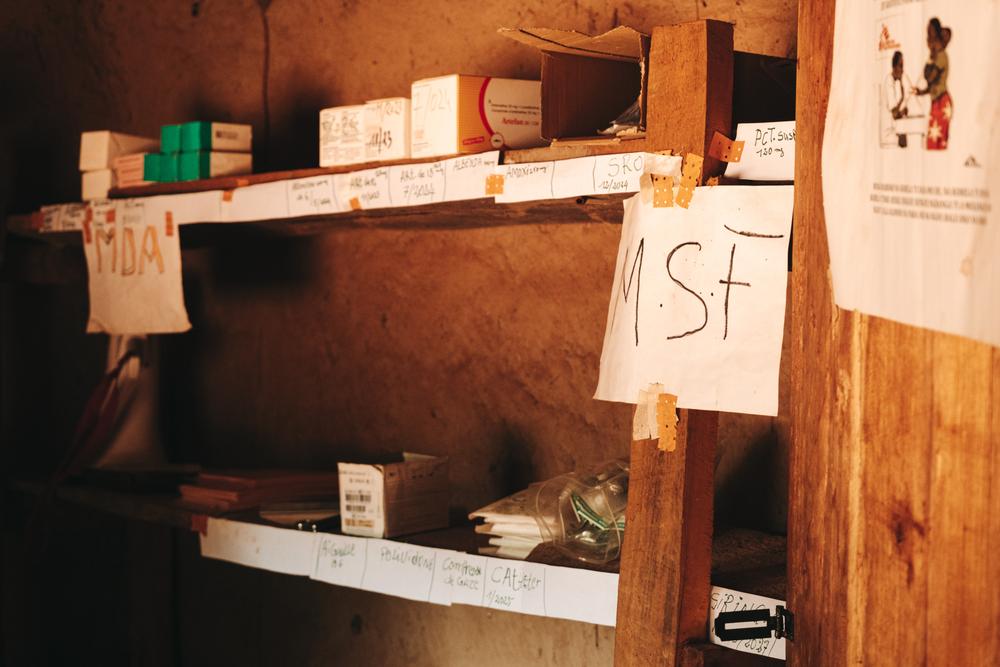
"For 12 years, not a single doctor was present here," he explains. "The hospital was run by a health assistant. Well, when I say 'hospital,' that's a big word. There is no electricity, no ambulance, and beds without mattresses. When I arrived, there wasn't even a thermometer, blood pressure monitor, pulse oximeter, or glucometer. The pharmacy was empty, too."
Although secondary hospitals like Bakouma hospital are supposed to provide more advanced care than health posts, health centers, and district hospitals, Dr. Louis-Marie Sabio struggles to provide even basic care. The hospital is empty and eerily silent. Despite the hospital’s size, there are fewer than10 patients. Chickens roam the corridors and wards, weaving between broken scales and rusty tables. Except for the vaccinations and referrals provided by MSF, the facility receives no other support. Patients know that despite Dr Sabio’s goodwill, the lack of human and material resources mean that they are unlikely to find the medical help they need.
"There are 18 of us running the hospital, but I'm the only one with medical training," said the young doctor. "Due to our limited technical resources, we can't meet the basic requirements of a hospital. We have no electricity, preventing us from performing ultrasounds or X-rays. The operating theater is virtually bare, equipped only with a small solar panel to power two light bulbs. When patients need medicines, we have to send them to the local market and hope they find something."
A critical health situation
This picture of no supplies, no staff, and no support is replicated in health facilities across the Central African Republic. According to a recent report from the World Health Organization (WHO) and the Ministry of Health, less than half of the country's healthcare facilities are fully operational1, and the ratio of doctors to people is alarmingly low, with only 0.6 doctors for every ten thousand people – one of the lowest in the world.
Decades of political unrest and violence among armed groups fueled a massive crisis, leaving more than half of the country's six million citizens in need of humanitarian aid. The country's life expectancy is a mere 54 years. Pregnant women face a substantial risk of death or severe illness due to the scarcity of gynecologists. And child mortality rates rank among the highest globally.2.
"We often feel alone"
MSF has nearly 2,800 staff members in the country—it’s one of our largest programs across the 75 countries we work in. Most hired locally, they work tirelessly to support health authorities and communities improve access to healthcare in some of the most neglected areas. In the Mbomou prefecture, MSF supports fifteen health facilities, from small remote health posts to the Bangassou regional university hospital (HRUB)—the only specialized reference facility serving a region the size of Greece.
Initially launched as an emergency response to the massive violence that shook the country in 2013-2014, MSF's programs in this area now service a significant portion of the prefecture. MSF sends mobile teams to local health facilities to provide essential equipment, vaccines, and vital medicines that can help treat common childhood diseases in the region, such as malaria, diarrhea, and respiratory infections. MSF also provides training to health workers. Our teams also arrange referrals for patients in critical condition to Bangassou's hospital, where we support most lifesaving services.
"[Our] objective is to bolster healthcare provision at all levels to reduce mortality in the area," explains Pelé Kotho-Gawe, MSF's nurse supervisor for mobile activities in Bangassou.
However, the needs remain grossly neglected as MSF is not—and cannot be—everywhere. Humanitarian organizations are scarce in this region, even though violence has calmed somewhat in recent years. The lack of access to water and electricity in health facilities, on top of economic difficulties, exacerbates the massive health crisis, which MSF cannot address alone.
"We are confronted with realities that make this work seem endless,” said Kotho-Gawe. “We can treat children suffering from diarrhea, but without anyone drilling boreholes, the problem persists as [people] continue to drink untreated water. The same goes for malaria: We visit health centers where 90 percent of the tests are positive for malaria, and we provide free care for the children, but no one in the area is engaged in preventive measures or distributing mosquito nets. Sometimes other organizations come through, but they are not frequently seen, and we often feel alone in tackling these challenges. MSF clearly cannot handle everything on its own."
Bangassou hospital, a mirror of the ongoing crisis
As MSF’s team travels further into the region, from health post to health center, this feeling deepens. Without MSF’s assistance, pharmacy stocks would be depleted, parents would struggle to afford treatment for their children, and
However, this support is not enough, and Bangassou hospital is a stark reminder of this fact. The hospital is the last hope for all complications that cannot be treated elsewhere. In other words, patients flock to this facility day and night, sometimes traveling hundreds of kilometers by motorbike over rough terrain, because treatment or medications are not available elsewhere.
The other day, I had to make an emergency transfer of a baby to Bangassou by motorbike, as we don't have an ambulance. We couldn't stabilize him, and he died a few kilometers from here, on the motorbike" says Dr Louis-Marie Sabio
Four-year-old Guy arrived in a coma. He suffers from type 1 diabetes—a disease that requires lifelong injections of insulin. His parents brought him to Bangassou from Bao, more than 100 kilometers away, because the hospitals near his home did not have insulin.
Newborn René* was admitted for the third time to intensive care due to severe malnutrition, as the malnutrition prevention programs in Bangassou formerly run by an international nongovernmental organization (NGO) were discontinued.
Twenty-year-old Fanny was transferred from Bakouma, 130 kilometers away, because Dr. Louis-Marie Sabio and his team lacked the medicines and equipment needed to treat the wound on her back.
"In a normal situation, patients like Fanny should be treated at my hospital," said Dr. Louis-Marie Sabio, who was visiting Bangassou hospital for an MSF training session. "But you've seen the state of the facility I run. I still send patients to Bangassou who shouldn't need to be referred. Sometimes, I even have to refer patients without being able to stabilize them beforehand, unsure if they will survive. The other day, I had to make an emergency transfer of a baby to Bangassou by motorbike, as we don't have an ambulance. We couldn't stabilize him, and he died a few kilometers from here, on the motorbike."
Where is everyone
"The health situation in the CAR is shocking, but I'm almost as shocked by the lack of international attention paid to it," said René Colgo, MSF's head of mission in Central African Republic.
"Despite the scale of the crisis and the staggering statistics, the plight of [people] remains largely unknown to the outside world, and humanitarian funding for the country falls far short of the scale of the needs. For reasons linked to insecurity or logistical constraints, NGOs are not always present in the areas where the needs are greatest. Much more must be done to support people. Where is everyone? We cannot and must not get used to seeing CAR at the top of the worst humanitarian league tables."
To bring about change, it's high time to see the situation in the CAR for what it really is: a severe and lasting humanitarian crisis that requires the mobilization of everyone.
Does anybody care
Watch the documentary "Does anybody care", which reflects the reality of a country suffering from both a flagrant lack of access to healthcare and a lack of attention and support for its people from the international community.
1HeRAMS reference report, WHO/Ministry of Health, 2023
2World Bank, statistics on maternal and infant mortality, available at https://donnees.banquemondiale.org
3https://www.care-international.org/resources/breaking-silence-report-ten-humanitarian-crises-didnt-make-headlines-2022